Local corticosteroid injections are widely used for short-term pain relief and to help facilitate rehabilitation for patients with shoulder pain. The most common injections carried out in clinic are into the sub-acromial (SA) bursa, the glenohumeral (GHJ), the long head of biceps (LHB) and the acromio-clavicular (ACJ) joint. On occasion a suprascapular nerve block may also be carried out for pain relief. The indications for each injection vary and are based on clinical examination and investigations.
Ultrasound (US) is a safe, effective imaging tool to guide musculoskeletal injections into the intended anatomical space. US has the unique advantage of being able to visualise soft tissues, bony landmarks, and the needle with real-time scanning, thereby allowing dynamic visualisation. US guided injections have become more popular because of the recent advances in image quality, decreased cost of use, portability and lack of radiation exposure.
Research into guided versus unguided (or landmark/anatomical guided) injections focuses on two main areas; accuracy and efficacy. There is a significant body of evidence to suggest that unguided injections are inaccurate and shoulder injections are no exception. For all shoulder injections studies have demonstrated that needle placement is more accurate with image guidance.
The accuracy of unguided injections is generally poor. We know that 14% to 71% of unguided injections miss their target and the use of US guidance significantly decreases failure rates to about 5% (Finnoff et al, 2014). It is more controversial whether accuracy of needle placement determines clinical outcomes. Many studies have demonstrated improvement in shoulder symptoms irrespective of whether the needle was in the targeted structure or not. Others have reported improved clinical outcome with image-guided injections (Abdel-Rahman Aly et al, 2014).
Henkus et al (2006) reported that 62.5 to 76% of unguided SA injections reached the intended target. Injections isolated to the SA bursa resulted in significantly decreased pain and improved functional scores, whereas injection of other structures resulted in increased pain scores. Eustace et al (1997) reported an accuracy rate of 29% (4 of 14) of unguided SA and 42% (10 of 24) of glenohumeral joint injections . There was also a positive correlation between clinical outcome and accurately placed injections. LHB injections have been shown to reach the intended target only 27% of the time (Hashiuchi et al, 2011). One of the most superficial injections carried out is an AC joint injection, but even their accuracy varies from 33-72% for unguided procedures compared with 90-100% in guided procedures (Finnoff et al, 2014) (Figure 1).
Figure 1 - US guided ACJ injection using a transverse in-plane approach
Soh et al (2011), in a large systematic review assessed the efficacy of all shoulder injections (GHJ, SAB, ACJ and LHB) and showed a statistically significant greater improvement in shoulder pain and function at 6 weeks after injection, and also had less adverse events.
The literature in this area still lacks high quality research to help guide our clinical practice. Short follow ups, lack of blinding and small sample sizes are some of the limitations in the current literature. More adequately powered and well-executed randomised controlled trials are required.
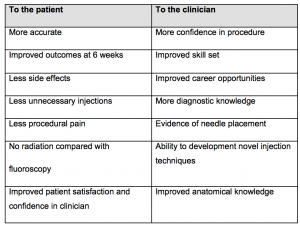
Without guidance more advanced shoulder techniques such as lavage/barbotage and hydrodistention are not possible. These can be carried out under fluoroscopy however are expensive and expose the patient to radiation. US guidance would appear to be the imaging of choice for all guided shoulder procedures. There are other advantages to using US guidance other than the accuracy and efficacy debate (Table 1).
Table 1: Advantages of US guided injections
Is it difficult to learn?
Carrying out a guided injection is a technical skill, which requires extensive practice to refine and perfect. It is essential that clinicians who want to learn guided injections gain a basic level of US probe skills and knowledge beforehand. Interestingly, in one cadaveric study students with no experience in imaging successfully infiltrated the AC joint with only minimal supervision beforehand (Sabeti-Aschraf et al, 2011).
Conclusion
US guided injections have gained extensive use over the last few years, particularly in the hands of non-radiologists, replacing the traditional unguided approach. US guided injections have been shown to improve accuracy and efficacy compared with unguided injections. There are many advantages to the clinician and the patient. Adding US and US guided injections to your practice significantly improves your:
• Diagnostic capabilities
• Anatomical knowledge
• Patient pathways – advent of ‘one stop clinics’
• Pathological knowledge
• Clinical reasoning skills
• Job opportunities
• Decision-making and management skills
But more importantly it allows for an early and accurate diagnosis, which is essential for the implementation of a timely and effective treatment plan for your clients.
If you have any questions please email chris@ultrasoundtraining.co.uk or visit www.ultrasoundtraining.co.uk
Reference List:
Aly, A. R., Rajasekaran, S., & Ashworth, N. (2015). Ultrasound-guided shoulder girdle injections are more accurate and more effective than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med, 49(16), 1042-1049.
Eustace, J. A., Brophy, D. P., Gibney, R. P., Bresnihan, B., & FitzGerald, O. (1997). Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Annals of the Rheumatic Diseases, 56(1), 59-63.
Finnoff, J. T., Hall, M. M., Adams, E., Berkoff, D., Concoff, A. L., Dexter, W., & Smith, J. (2015). American Medical Society for Sports Medicine position statement: interventional musculoskeletal ultrasound in sports medicine. Clinical Journal of Sport Medicine, 25(1), 6-22.
Hashiuchi, T., Sakurai, G., Morimoto, M., Komei, T., Takakura, Y., & Tanaka, Y. (2011). Accuracy of the biceps tendon sheath injection: ultrasound-guided or unguided injection? A randomized controlled trial. Journal of shoulder and elbow surgery, 20(7), 1069-1073.
Henkus, H. E., Cobben, L. P., Coerkamp, E. G., Nelissen, R. G., & van Arkel, E. R. (2006). The accuracy of subacromial injections: a prospective randomized magnetic resonance imaging study. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 22(3), 277-282.
Sabeti-Aschraf, M., Lemmerhofer, B., Lang, S., Schmidt, M., Funovics, P. T., Ziai, P., ... & Schueller-Weidekamm, C. (2011). Ultrasound guidance improves the accuracy of the acromioclavicular joint infiltration: a prospective randomized study. Knee Surgery, Sports Traumatology, Arthroscopy, 19(2), 292-295.
Soh, E., Li, W., Ong, K. O., Chen, W., & Bautista, D. (2011). Image-guided versus blind corticosteroid injections in adults with shoulder pain: a systematic review. BMC musculoskeletal disorders, 12(1), 137.