Musculoskeletal (MSK) ultrasound is a rapidly developing and in-demand technique which is increasingly recognised as a valuable diagnostic tool, having several advantages over magnetic resonance imaging (MRI). Over the past decade the usage and application of diagnostic ultrasound in MSK and sports medicine has developed significantly. Between 2000-2009 there was 717% increase in the number diagnostic ultrasound scans carried out (Smith et al., 2009). A majority of these were carried out by non-radiologists.
Ultrasound is the new stethoscope (BJSM, 2010)
Why ultrasound and why now?
There are many reasons for the increase in the use of diagnostic ultrasound in MSK medicine (Article: Top 10 reasons for using ultrasound). Over the past decade there has been significant technological advances in the machines, they have become smaller and more portable and their price has reduced! It is now possible to get a portable machine for approximately £12,000 to £45,000 for example the GE LOGIQ, which (in the right hands!) can produce excellent images that would now out perform any of the large, more expensive hospital based machines 10 to 15 years ago. The development of transducer technology has allowed the demonstration of soft-tissue architecture at a superior spatial resolution to MRI (Figure 1) (Smith & Miader, 2007). Despite these developments the prices have not gone up, in fact they have gone down! (Article: What to look for when purchasing an ultrasound scanner). This has made the machines more affordable and accessible to a range of clinicians who are starting to realise the many benefits of combining their clinical assessment with a diagnostic scan.
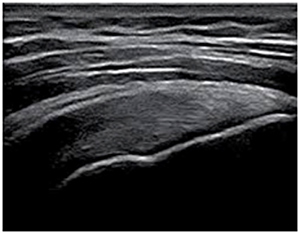
Figure 1: Longitudinal view of the supraspinatus tendon. You can clearly see the fibrillar pattern of the tendon fascicles. High frequency linear transducers, compound imaging, tissue harmonic imaging, and extended-field-of-view, to name a few, have improved ultrasound imaging of joints and soft tissues.
Radiologists are the pioneers of diagnostic ultrasound and they have made significant advances in proving the diagnostic ability and applications of ultrasound over the past 20 years. For many soft-tissue lesions e.g. tendon, muscle and ligament injuries, ultrasound can now provide as much diagnostic information, or often more information, than MRI scans (Figure 2).
There is a chronic shortage of adequately trained radiologists and radiographers and an escalating demand for ultrasound examinations (Bates et al., 2003). This has produced an opportunity for non-radiologists to develop new ways of working and to carry out the scans themselves to help meet this demand.
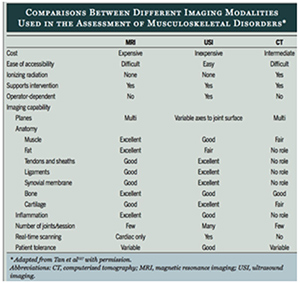
Figure 2: Comparison with the different imaging modalities used in MSK medicine (Tan et al., 2003)
Structure, Function and Pain
Over the past 10 years there has been a significant amount of research highlighting the disconnect between structural changes on imaging, the clients functional ability and pain. The classic phrase 'treat the patient, not the scan' springs to mind. Any imaging should be interpreted in a clinical context and so, if possible, the person who carries out the clinical examination would ideally perform the imaging.
It must be very challenging for radiologists to prioritise the importance of the imaging findings without having taken the full history and clinical examination. The risk is that clinically insignificant findings may be overemphasised and clinically relevant findings may be overlooked (Nazarian, 2008).
This issue is negated if the scan is carried out and the findings interpreted immediately as part of, and in conjunction with, the clinical examination. For this to occur 'clinicians' e.g. sports doctors, physiotherapists, orthopaedic surgeons, osteopaths and GP's need to develop their imaging skills (ultrasound & probe skills) and the 'radiologists' and 'sonographers' need to develop their clinical skills (Figure 3). This will ensure that whatever your professional background the result is 'clinically integrated ultrasound'. Recognition of ultrasound as a speciality would help to expedite national standards and competency guidelines whatever your professional background.
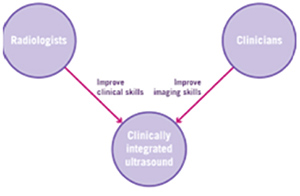
Figure 3: The goal is to achieve a 'clinically integrated ultrasound' irrespective of your professional background
One-stop clinics
Ultrasounds scanners are very portable and time-efficient, particularly when compared to MRI scans. For example, a shoulder scan to rule out a full thickness rotator cuff tear can take as little as 2 to 3 minutes in competent hands. Ultrasound lends itself well to combining the clinical assessment with imaging in clinic. It becomes a natural extension of your clinical assessment.
Full examinations by experts are being replaced with more focused scans by clinicians to answer specific questions formulated from the history and clinical findings. Such clinics, known as 'one-stop clinics', allow the clinician to carry out a clinical assessment, an ultrasound scan and if appropriate an ultrasound guided injection in one appointment. No referrals, no waiting lists, fewer appointments and immediate feedback to the client.
Shoulder, and foot and ankle clinics lend themselves very well to these 'one-stop clinics'. These reduce unnecessary waiting times and appointments and improves client satisfaction (Figure 4). This is one of the reasons we have seen a significant increase in the number of orthopaedic surgeons attending our courses. Over the past year we have taught several on-site courses specifically for orthopaedic surgeons wanting to learn how to scan and how to carry out ultrasound guided injections. We are also pleased to announce that for 2017 we have joined forces with the world renowned Mr. Len Funk, (www.shoulderdoc.com) to run an upper limb-specific ultrasound imaging and cadaveric ultrasound guided injection course.
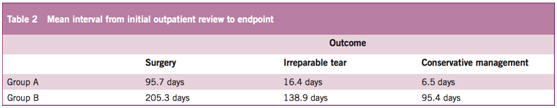
Figure 4: (Saegger et al, 2011) Shoulder 'one stop shop' - the use of a portable ultrasound machine by an orthopaedic surgeon (Group A) can significantly reduce the time to treatment and the financial cost associated with patients with rotator cuff tears.
Our courses attract a variety of clinicians from MSK and sports medicine. These include radiologists, sports medicine doctors, physiotherapists, A & E consultants, sonographers, orthopaedic surgeons, GP's, osteopaths and chiropractors.
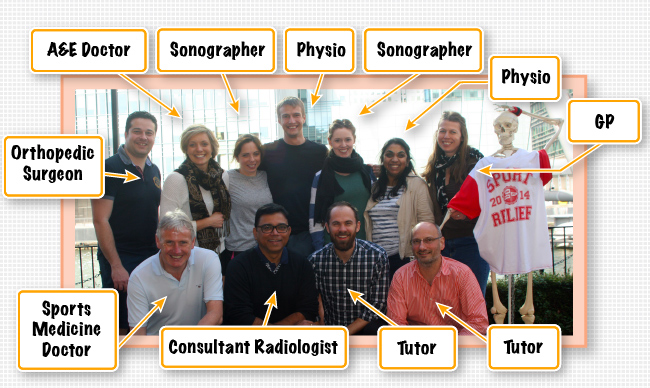
Delegates from our 2-day Introduction to Musculoskeletal Ultrasound course
MSK ultrasound is used in a variety of ways, by different professions. Our courses provide a unique and exciting learning environment where clinicians can interact, learn from each other and share their clinical thoughts and knowledge.
For further information please do not hesitate to contact us at info@ultrasoundtraining.co.uk