A 56 year old woman presented with an 18 year history of left ankle pain, clicking and instability. The onset was following a fall down approximately 8 steps and symptoms have been present to a greater or lesser degree since. The pain is aggravated by descending stairs, running, and changing gear. The instability is most noticeable when descending stairs and is causing the patient considerable anxiety as she has fallen downstairs on two further occasions. Magnetic Resonance Imaging (MRI) of the left ankle was performed in 2006 which demonstrated “bone marrow oedema in multiple bones of the foot and oedema within the subcutaneous tissues overlying the lateral aspect of the foot”. It also reported that the “medial and lateral ligamentous complexes are intact” and that “the tendons around the ankle joint are normal.” She has had various treatment interventions including physiotherapy, osteopathy, and surgery. She reported that the surgery (performed in 2007) was carried out to “remove a bone fragment” which stopped the ankle “locking” but did not improve the pain levels or instability.
On clinical examination there was no swelling, redness, or heat. A palpable click was elicited on ankle inversion, there was significantly reduced power on ankle eversion and the muscle belly of peroneus brevis appeared to be significantly reduced in size.
The most probable differential diagnosis for lateral ankle pain is lateral ligament injury, peroneal tendon injury, sinus tarsi syndrome and nerve entrapments.
An ultrasound scan (US) was performed using a Mindray MX-7 machine. A high frequency linear transducer (6-13MHz) was employed. A high frequency was selected as this is most suitable for scanning superficial structures. The gain was adjusted to provide the best resolution. Focus was set at the depth of the peroneal tendons. A spin manoeuvre was used to transition between transverse and longitudinal views. Assessment of the ankle was conducted with the patient seated on a treatment table with the knee flexed, and the ankle internally rotated. Transverse and longitudinal views of the lateral ankle and foot were taken and dynamic testing was used where appropriate. Dynamic testing included active circumduction of the ankle (as the patient was able to routinely reproduce the click in this manner) and passive dorsiflexion and inversion of the ankle. Lots of gel was used to compensate for the curve of the malleolus. On reflection, had one been available, using a hockey stick probe would probably have made it easier to scan the affected area and may have improved the quality of the images.
Report: “The superior peritoneal retinaculum appears to be of normal thickness and intact. Both peroneal tendons maintain their homogenous, fibrillar pattern and are of normal thickness. There is no fluid within the sheath. There is no evidence of neovascularisation on power Doppler. There is subluxation of the tendon of peroneus longus over peroneus brevis on ankle inversion with dorsiflexion. These findings are consistent with intrasheath subluxation of the peroneal tendons.”
Figure 1
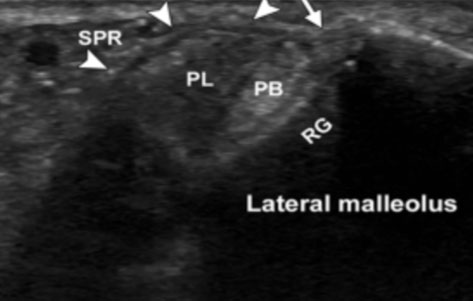
Figure 2
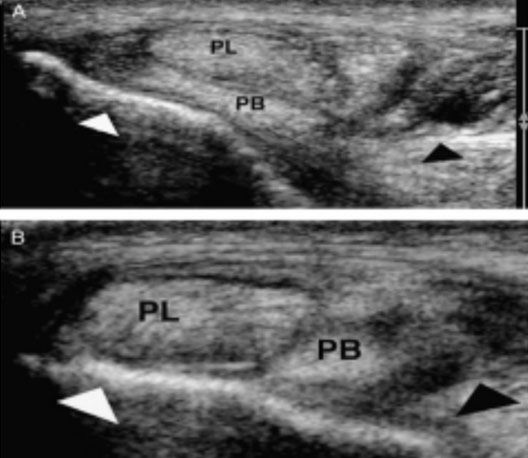
Figure 2 demonstrates US findings similar to our own.
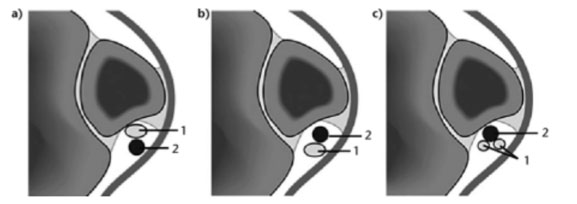
Our ultrasound findings combined with the clinical examination are suggestive of intrasheath subluxation of the peroneal tendons. Dislocation of the peroneal tendons out of the peroneal groove associated with a tear to or avulsion of the superior peroneal retinaculum (SPR) is well described in the literature. However, there is a subset of patients whose tendons sublux with an intact SPR. Intrasheath subluxation is reversal of the positions of the peroneus longus and brevis tendons (Raikin, Steven & Elias, Ilan & Nazarian, Levon., 2008). There are two types of intrasheath subluxation as shown in Figure 3. Type A subluxation is the switching of anatomical position of intact tendons. Type B is the subluxation of peroneus longus through a longitudinal split in peroneus brevis. In the absence of evidence of a longitudinal tear in peroneus brevis, it would be reasonable to suggest that this is a Type A subluxation.
Figure 3
Intrasheath subluxation is not widely reported and, its exact incidence appears unknown (Draghi, F., Bortolotto, C., Draghi, A.G. and Gitto, S. 2018). Its aetiology has been reported as being associated with a low-lying peroneal muscle belly or the presence of a peroneus quartus muscle and tendon (Thomas et al, 2009). Raikin et al reported that out of 14 patients that underwent surgery, it was discovered intraoperatively that 13 had convex peroneal grooves.
Ultrasound was first used medically in 1942 to locate brain tumours (Newman and Rozycki. 1998). Although used in prenatal examination during the 1960s in 1972 the first ultrasound
images of human joint were published. High-resolution ultrasound has improved the quality of images allowing accurate interpretation and diagnosis. Ultrasound units work by providing an electrical charge to piezoelectric crystals in the transducer. This produces the soundwaves that bounce off structures in the body returning to the transducer and converted into images (D. Kane, W. Grassi, R. Sturrock, P. V. Balint., 2004).
Ultrasound is incredibly safe, it is the only imaging modality readily used on foetuses in utero (Adler, Sofka and Positano, 2004). There is a risk regarding the amount of heat energy created while scanning. The risk is of increased heat caused by cavitation from the ultrasound waves. The British Medical Ultrasound Society suggests during extended time scanning with Doppler the increase can be 4°C+ which could be harmful to a foetus. This is not overly concerning in musculoskeletal (MSK) clinics.
US is a key method of diagnosis together with clinical findings. It is safe and inexpensive compared to MRI. It has been shown 31% of musculoskeletal (MSK) diagnoses made with MRI could have been made with US, such is the saving with ultrasound that in the USA it could have saved $6.9 billion over 15 years (Jacobson, 2009). MRI is contraindicated in patients with pacemakers and some metal implants. Some patients will refuse MRI as they are claustrophobic. US has none of these limitations.
In this instance ultrasound was instrumental in arriving at an accurate diagnosis as we were able to perform dynamic testing of the injured area. It has been stated that dynamic ultrasound is the imaging modality of choice for evaluating intrasheath subluxation of the peroneal tendons (Draghi F et al, 2018). The same authors suggest that this condition is commonly missed on physical examination alone because of the lack of tendon displacement over the lateral malleolus. The palpable (and audible) click the patient had reported was reproducible by dorsiflexing and everting the ankle both actively and passively. As a result, we were able to capture still and video images of the peroneus longus brevis tendons as they switched anatomical positions. US also offers the advantage of allowing patient feedback via sonopalpation. Sonopalpation allows the clinician to use US in combination with physical examination and gives the ability to localise pain and relate it to specific structures anatomically (Faust, J.S., Tsung, J.W., 2017). We also determined that the SPR appeared intact; that there was no evidence of neovascularisation (via Doppler) and that there was no evidence of tears in either tendon. It has been suggested that US is 90% accurate in the diagnosis of peroneal tendon tears (Grant TH, Kelikian AS, Jereb SE, McCarthy RJ., 2005) and dynamic US has been reported as 100% accurate in the diagnosis of intrasheath subluxation with an intact SPR (Raikin et al, 2008). There appears to be little further information in the literature regarding the specificity and sensitivity of either US or MRI with relation to intrasheath subluxation. Rockett et al (1998) performed a study on 28 patients who underwent surgery for tendon disorders around the ankle. The intraoperative findings were compared with preoperative US findings in all 28 patients and preoperative MRI findings in 20 of those same patients. From this data they calculated the sensitivity, specificity and accuracy for both modalities. It was suggested that US was 100% sensitive, 89.90% specific and 94.4% accurate in the detection of ankle tendon tears. This compares with figures of 23.4% sensitivity, 100% specificity and 65.75% accuracy for MRI. US appears markedly more sensitive and accurate in the detection of ankle tendon tears and it may be the case that this also true of intrasheath subluxations however, more work is probably required to assess the relative merits of US and MRI.
Computerised Tomography (CT) may be may be used to detect bony abnormalities such as avulsion and fractures, it may also show tendons which have dislocated from the peroneal groove and/or tendinopathy (Kumar Y, Alian A, Ahlawat S, Wukich DK, Chhabra A., 2017). However, these findings are not commonly associated with intrasheath subluxation as there is often no evidence of bony injury or tendinopathy and the tendons remain the peroneal groove. There are relatively few contraindications to CT although it should be avoided in pregnant patients, especially those in the first trimester. Unlike US and MRI, CT involves the patient receiving a dose of radiation. According to Ludlow (2018) the amount of radiation exposure for an adult undergoing ankle/foot CT imaging ranges between 0.3 and 4.6 micro Sieverts compared to 0.001 to 0.06 for a 2D radiograph. At the higher end this is equivalent to approximately 18 months of exposure to natural sources of radiation. Power et al (2016) stated that “the association between low-dose radiation (of the order used in standard diagnostic examinations) and oncogenesis is unclear.” However, the same authors also remarked that “there is an inherent responsibility on the medical community to keep radiation doses as low as reasonably achievable”.
Subsequent to our US evaluation the patient was referred (by an orthopaedic surgeon) for MRI of the foot and ankle. The report from the MRI was unremarkable showing that the “peroneal tendons lie in normal position and are intact with no tear synovitis”. This confirmed our findings in terms of there being no tearing of either peroneal tendon, no fluid or swelling, or disruption to the SPR. The significant limitation of MRI in this instance was the inability to perform any sort of dynamic evaluation. Most commonly MRI is performed with the patient supine and the ankle in a neutral position with about 20 degrees of plantar flexion (Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD., 2015). In instances of peroneal tendon injury, the advantage of MRI is that it allows assessment of the articular cartilage and bone marrow (Lee, S.J., Jacobson, J.A., Kim, SM. et al., 2013).
However, US allows comparison with the other side and is the best modality for detecting transient events such as subluxation (Bianchi S, Delmi M, Molini L., 2010).
US is far more accessible than either MRI or CT. Advances in US technology have made it possible for US imaging to be performed in a wide variety of clinical settings at the “chair side” or, indeed, pitch-side. The same advances in technology have reduced the price portable US machines which has made the cost of accessing these services much more palatable. By contrast, both MRI and CT are most commonly found within a hospital or specialist private setting and, consequently, are somewhat less accessible than US. Having said that, the advent of multiple private providers has made referral for MRI much more straightforward and accessible. High quality images and reports are often available within a matter of days from referral. There are some limitations to US. There is a relatively limited field of view determined by the footprint of the transducer, there can be limited penetration in obese patients and US cannot penetrate bone. The quality of the images obtained and their subsequent interpretation is also dependent on a number of factors. These include the anatomical knowledge of the clinician, their scanning skill and experience and their ability to interpret the images. The quality of US machines is also somewhat variable and this can have a significant impact on the images produced.
I would argue that MRI added little to our understanding of this patient’s condition other than providing confirmation of some of our findings and demonstrating the absence of other possible findings such as bone marrow oedema, osteochondral lesions and other ankle pathologies.
Most peroneal tendon lesions can be treated conservatively using physical therapy, activity modification, non-steroidal anti-inflammatory medications (NSAIDs), changing footwear, temporary immobilisation and corticosteroid injections (Frederick Michels, Stéphane Jambou, Stéphane Guillo, Jan Van Der Bauwhede., 2013). However, as in this instance, where 3 to 6 months of conservative treatment has failed, surgery is indicated. Indeed, it has been suggested that there is a limited role for conservative management (Raikin and Fox, 2020). This patient has had various investigations and has tried a variety of approaches since the initial injury in 2003. She had consulted multiple physical therapists, seen her GP on numerous occasions and undergone surgery. Despite this she had not received a clear diagnosis and all attempts to treat or rehabilitate her ankle had failed. When she consulted us, we were able to give her considerable insight into her condition via thorough history taking, clinical examination and US. US proved invaluable as we were able to reproduce the subluxation whilst imaging the affected area. On this basis and the past history of failed management, both conservative and surgical, we referred the patient to a local foot and ankle surgeon for their opinion. He ordered MRI which was unremarkable. His clinical examination, in combination with our report detailing our clinical and US finding, led him to advise surgery. Surgical options include peroneal groove deepening with retinacular reefing and repairing tendon tears (Raikin, 2009). This approach can involve extensive opening of the area to facilitate visualisation of the tendons, this can be associated, post-operatively, with scar formation and sural nerve entrapment (Sammarco, 2009). Michels et al (2013) have suggested that an endoscopic approach has a number of advantages and good outcomes. The theory is that a significant cause of subluxation is low-lying fibres of the peroneal muscles which increases the compressive forces within the fibro-osseus tunnel of the peroneal groove. They recommend debriding or resecting the low-lying muscle fibres to reduce those forces. The same authors did not recommend any peroneal groove deepening. Indeed, it has been suggested that a convex peroneal groove is not a pathologic finding as the groove is not formed by concavity of the fibula rather a thick ridge of fibrocartilage along the posterolateral lip of the distal fibula (Ferran and Muffulli, 2008). It is unknown at this point which approach the patient’s surgeon is going to use.
There is relatively little literature on intrasheath peroneal tendon subluxation, both in terms of diagnosis/imaging and management. Many studies involve small patient numbers as the condition is relatively rare. This is contrasted with significant amounts of literature regarding dislocation of the peroneal tendons out of the peroneal groove. However, it would appear that surgical outcomes are largely successful. Michels et al reported that the 3 patients in their study were allowed to mobilise and fully weight-bear immediately and they all started physiotherapy from 5 days after surgery. They were all pain free and had no snapping sensation at 2 months post-surgery and at 2 years post-surgery they all had normal function and no complaints. Raikin et al’s study involved 14 patients who underwent peroneal groove deepening with retinacular reefing. At 24 months post-surgery 13 of the 14 no longer had a demonstrable, persistent subluxation and the average score on the visual analogue pain scale was down to 1.2 from 6.8.
On this occasions US was invaluable in forming an accurate diagnosis. We were able to confirm our clinical findings using dynamic testing at the time of the initial consultation. This proved very beneficial for our patient as US proved a very convenient, low cost and accurate modality to use. She was then able to obtain a very rapid referral to an orthopaedic surgeon via her GP. It could be argued that, had she undergone US examination at an earlier date, she might have received a more accurate diagnosis and avoided some of the failed interventions. It is unknown whether this delay in arriving at a diagnosis and receiving appropriate treatment will affect recovery and the eventual outcome. It has been demonstrated that US is highly sensitive and accurate in diagnosing ankle tendon injuries. Further research is needed both in terms of imaging modalities and surgical approaches in the specific case of intrasheath peroneal tendon subluxation. Upon reflection it may have been useful to have used a hockey stick probe as this would potentially have allowed for easier scanning of the area and produced better quality images. This case highlighted the need for some practise in the skill of performing dynamic testing whilst maintaining the position of the transducer and also revealed some gaps in anatomical knowledge.
Thomas JL, Lopez-Ben R, Maddox J. A preliminary report on intra-sheath peroneal tendon subluxation: a prospective review of 7 patients with ultrasound verification. J Foot Ankle Surg. 2009 May-Jun;48(3):323-9.
Draghi, F., Bortolotto, C., Draghi, A.G. and Gitto, S. (2018), Intrasheath Instability of the Peroneal Tendons: Dynamic Ultrasound Imaging. J Ultrasound Med, 37: 2753-2758.
Grant TH, Kelikian AS, Jereb SE, McCarthy RJ. Ultrasound diagnosis of peroneal tendon tears. A surgical correlation. J Bone Joint Surg Am. 2005 Aug;87(8):1788-94.
Raikin, Steven & Elias, Ilan & Nazarian, Levon. (2008). Intrasheath Subluxation of the Peroneal Tendons. The Journal of bone and joint surgery. American volume. 90. 992-9. 10.2106/JBJS.G.00801.
Rockett MS, Waitches G, Sudakoff G, Brage M. Use of ultrasonography versus magnetic resonance imaging for tendon abnormalities around the ankle. Foot Ankle Int. 1998 Sep;19(9):604-12.
Jacobson J. Fundamentals of Musculoskeletal Ultrasound. 2018
Kumar Y, Alian A, Ahlawat S, Wukich DK, Chhabra A. Peroneal tendon pathology: pre-and post-operative high resolution US and MR imaging. Eur J Radiol. 2017 Jul;92:132-144.
Ludlow JB. Hand-wrist, knee, and foot-ankle dosimetry and image quality measurements of a novel extremity imaging unit providing CBCT and 2D imaging options. Med Phys. 2018 Nov;45(11):4955-4963.
Power SP, Moloney F, Twomey M, James K, O'Connor OJ, Maher MM. Computed tomography and patient risk: Facts, perceptions and uncertainties. World J Radiol. 2016 Dec 28;8(12):902-915.
Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD. High-resolution US and MR imaging of peroneal tendon injuries. Radiographics. 2015 Jan-Feb;35(1):179-99.
Bianchi S, Delmi M, Molini L. Ultrasound of peroneal tendons. Semin Musculoskelet Radiol. 2010 Sep;14(3):292-306.
Frederick Michels, Stéphane Jambou, Stéphane Guillo, Jan Van Der Bauwhede. Endoscopic Treatment of Intrasheath Peroneal Tendon Subluxation. Case Reports in Medicine, vol. 2013, Article ID 274685, 4 pages, 2013.
Raikin S.M., Fox R. (2020) Intrasheath Subluxation of the Peroneal Tendons. In: Sobel M. (eds) The Peroneal Tendons. Springer, Cham.
Sammarco, Vincent James. Peroneal Tendoscopy: Indications and Techniques. Sports Medicine and Arthroscopy Review 17 (2009): 94-99.
Ferran NA, Oliva F, Maffulli N. Recurrent subluxation of the peroneal tendons. Sports Med. 2006;36(10):839-46.
Faust, J.S., Tsung, J.W. Eliciting renal tenderness by sonopalpation in diagnosing acute pyelonephritis. Crit Ultrasound J 9, 1 (2017).
Newman PG, Rozycki GS. The history of ultrasound. Surg Clin North Am. 1998 Apr;78(2):179- 95.
Adler, R., Sofka, C. M., Positano, R. G., 2004. Atlas of Foot and Ankle Sonography. Lippincott, Williams & Wilkins.
Lee, S.J., Jacobson, J.A., Kim, SM. et al. Ultrasound and MRI of the peroneal tendons and associated pathology. Skeletal Radiol 42, 1191–1200 (2013).